Assessment of Lung Sounds
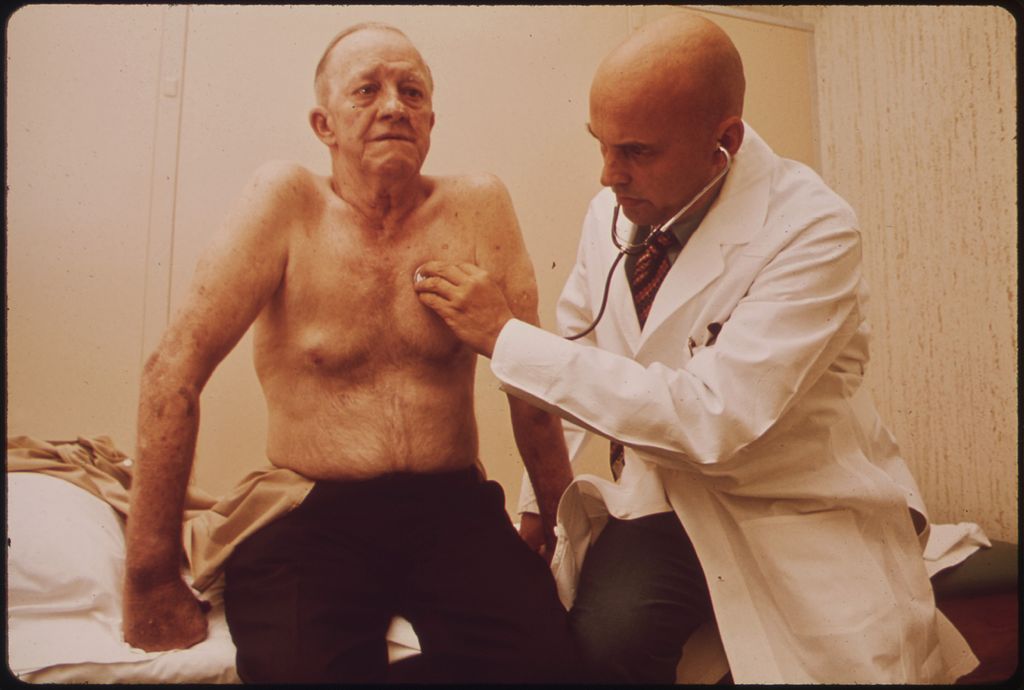
EMTs and Paramedics will routinely have to listen to and identify lung sounds. A good stethoscope is all that is required and the sounds that are heard during patient assessment can give the first responder clues as to what is going on with the patient during a respiratory emergency.
Medscape.com has a great explanation of the proper procedure in assessing lung sounds complete with a short video showing the proper assessment techniques. This can be found at: http://emedicine.medscape.com/article/1894146-overview.
For a full Stethoscope Buying Guide please visit: https://emttrainingstation.com/best-stethoscopes/
This article will cover 8 of the most common lung sound an EMT or Paramedic can expect to encounter as well as what they are usually indicative of.
1: Clear Normal Lung Sounds
Clear lung sounds are normal. This is what a patient should sound like upon inspiration and exhalation during normal healthy breathing.
2: Absent Lung Sounds
I really hope that you didn’t listen to this entire recording of nothing. Absent lung sounds are exactly what they sound like. Absent. First responders will not hear anything.
There is no air moving through the bronchioles, no gas exchange in the alveoli. Absent lung sounds mean that a patient is in respiratory arrest and rescuers should begin assisted ventilation with a BVM. Paramedics should consider immediate endotracheal intubation.
3: Diminished Lung Sounds
Absent or decreased sounds can mean air or fluid in or around the lungs, increasing the thickness of the chest wall, over-inflation of a part of the lungs, or reduced airflow to part of the lungs.
These will sound quieter than typical respirations. They can occur in both lungs or only one. Some examples of emergencies that can present with diminished lung sounds are: Pneumothorax, Hemothorax, Lung Cancer, Pleural Effusion, and Pneumonia.
4: Wheezing
Wheezing occurs when the upper airways become narrowed. This results in a high pitched sound, usually upon exhalation, as air is forced to go through tighter passages.
Wheezing is common in most respiratory ailments including: Asthma, Bronchitis, COPD, Allergies, ETC. Treatment for Wheezing usually involves administering a medication that either decreases inflammation or drys up excess secretions. These medications are typically given together.
Paramedic level providers can give medications such as: Albuterol, Atrovent, and Solumedrol. Basic EMTs will most likely treat wheezing with O2 and if a patient has their own prescribed inhaler, an EMT can assist with administration.
5: Rhonchi
Rhonchi is characterized by a low-pitched almost snoring type sound. It is attributed to secretions or obstructions in the upper and larger airways. This site, http://www.practicalclinicalskills.com/rhonchi.aspx, states that it is usually a symptom of: pneumonia, chronic bronchitis, cystic fibrosis, or COPD (chronic obstructive pulmonary disease).
The site also states that symptoms can be relieved through coughing. Rhonchi is a condition that can require medical intervention. Basic level care will include O2 therapy, whereas Paramedic level care can involve similar respiratory drugs as wheezing.
6: Crackles (Rales)
Crackles are caused by the explosive opening of small airways. Crackles are much more common during the inspiratory than the expiratory phase of breathing, but they may be heard during the expiratory phase.
Crackles are often associated with inflammation or infection of the small bronchi, bronchioles, and alveoli. Crackles that do not clear after a cough may indicate pulmonary edema or fluid in the alveoli due to heart failure, pulmonary fibrosis, or acute respiratory distress syndrome.
Crackles that partially clear or change after coughing may indicate bronchiectasis.
- Crackles are often described as fine, medium, and coarse. They can also be characterized as to their timing: fine crackles are usually late-inspiratory, whereas coarse crackles are early inspiratory.
- Fine crackles are soft, high-pitched, and very brief. This sound can be simulated by rolling a strand of hair between one’s fingers near the ears, or by moistening one’s thumb and index finger and separating them near the ears. Their presence usually indicates an interstitial process, such as pulmonary fibrosis or congestive heart failure. The sounds from interstitial pulmonary fibrosis have been described as sounding like opening a Velcro fastener.
- Coarse crackles are somewhat louder, lower in pitch, and last longer than fine crackles. Their presence usually indicates an airway disease, such as bronchiectasis.
They can also be described as unilateral or bilateral, as well as dry or moist/wet.
Source- https://en.wikipedia.org/wiki/Crackles
7: Pleural Rub
Pleural rub occurs then the lung is actually rubbing against the ribs. Normally there is a space between the lungs and rib cage called the pleural space. Common causes of pleural rub are pneumonia, pulmonary embolism, and pleurisy. They will appear upon exhalation and inhalation.
8: Stridor
Stridor is a high-pitched, almost whistling, sound. It associated with narrowing of the airways and is typically heard even without a stethoscope. According to Medscape:
Stridor is a symptom, not a diagnosis or a disease, and the underlying cause must be determined. It may be inspiratory (most common), expiratory, or biphasic, depending on its timing in the respiratory cycle, and the three forms each suggest different causes, as follows:
-
Inspiratory stridor suggests a laryngeal obstruction
-
Expiratory stridor implies tracheobronchial obstruction
-
Biphasic stridor suggests a subglottic or glottic anomaly
In most cases of stridor, besides a complete history and physical examination, along with other possible additional studies, flexible or rigid endoscopy is required for an adequate evaluation of the etiology.
For further information on Stridor visit: http://emedicine.medscape.com/article/995267-overview.
Stridor is a serious concern because it indicates an obstruction. EMS providers should check to make sure there is no visible foreign body in the throat and if needed follow protocols for extraction.
Stridor is common in children with Croup and epiglottis. The airway should be monitored and EMTs and Paramedics should be prepared to maintain the airway.
Conclusion:
If this post has been helpful to you then please like, share, and/or comment below. Remember this is meant to supplement not supplant classroom instruction or protocol. Always listen to instructions and follow local protocols when dealing with respiratory and airway emergencies.