Welcome to an in-depth exploration of the cardiovascular system and its significance in the field of emergency medical services. As an Emergency Medical Technician (EMT), your knowledge of this intricate system, the conditions that can arise, and the interventions necessary to save lives is fundamental to your role.
This comprehensive guide titled ‘The Cardiovascular System: EMT Interventions for Heart Conditions’ is designed to deepen your understanding and equip you with the practical knowledge you need in your life-saving work. In this five-part series, we will journey through the intricacies of the cardiovascular system, delve into the most common heart conditions you’ll encounter as an EMT, review essential interventions, and underline the importance of patient education in preventing cardiovascular disease.
Whether you’re a seasoned veteran in emergency medical services or an aspiring EMT just starting your career, this guide offers invaluable insights that will enhance your skills and enrich your professional journey. Let’s dive in and unravel the complexities of the cardiovascular system and the crucial role you play as an EMT in managing heart conditions.
This article is for informational purposes only and is NOT a replacement for proper education and training.
Table of Contents
Cardiovascular Anatomy: Understanding the Bodies Central Pump
The cardiovascular system, also called the circulatory system, is a complex biological network necessary for life. The cardiovascular system, which includes the heart, blood vessels, and blood, works tirelessly to supply oxygen and nutrients to all body cells and remove waste.
The heart is located centrally in the body. The heart is a relatively small muscle—about the size of a fist—but it has the enormous task of distributing blood throughout the body. The heart’s four chambers (two atriums and two ventricles) coordinate their contractions and relaxations to keep the heart beating at a steady rate. Blood is pumped out of the heart by the ventricles after being received by the atria. As a result of this cycle, blood is either oxygenated in the lungs (via the pulmonary circuit) or transported throughout the body (via the systemic circuit).
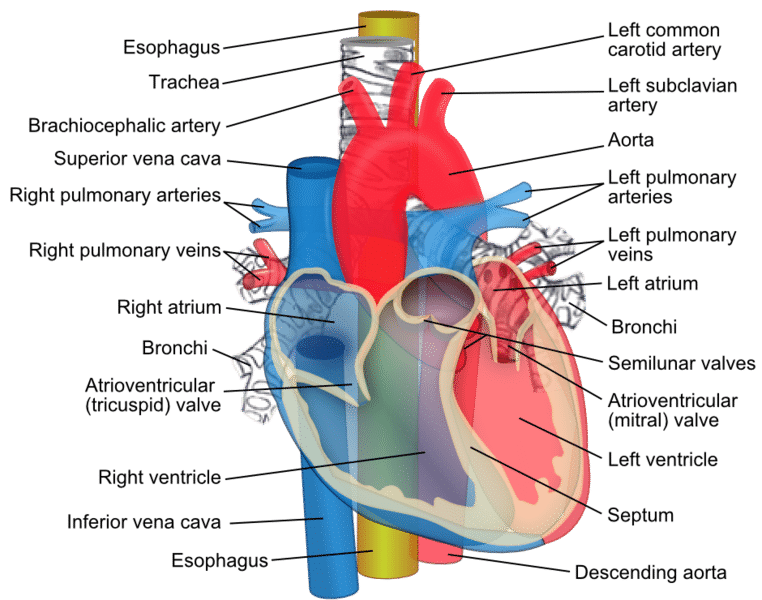
Take a moment to get to know the following anatomical structures of the heart as well as their functions
Anatomical Structures of the Heart:
- Vena Cava: The Vena Cava are divided into the superior and inferior vena cava. Together they are the largest veins in the human body. The superior (meaning above) vena cava brings deoxygenated blood mainly from the upper portions of the body such as the brain. The inferior (meaning below) vena cava brings deoxygenated blood from the lower portions of the body such as the legs and gut. This blood is carried to the heart so that is can be recirculated and reoxygenated before re-entering the circulatory system.
- Right Atrium: Acts as a deposit site for the Vena Cava. Blood in the right atrium is deoxygenated and will be pumped into the Right Ventricle.
- Tricuspid Valve: Named for having three flaps, this is the valve separating the right Atrium and Ventricle and is and one of two atrioventricular valves. This valve is open while the heart is in diastole.
- Right Ventricle: Part of the primary pumping force of the heart. Ventricles are responsible for pumping the blood out of the heart. The Right ventricle pushes blood through the pulmonic valve into the pulmonary arteries.
- Pulmonic Valve: This valve opens while the heart is in systole and allows blood to enter the pulmonary arteries.
- Pulmonary Arteries: The only arteries that carry deoxygenated blood. These blood vessels bring the blood from the heart to the lungs where an exchange of gases takes place.
- Pulmonary Veins: The only veins that carry oxygenated blood. These blood vessels bring blood from the lungs to the heart. The oxygenated blood is now ready for redistribution throughout the rest of the body.
- Left Atrium: Acts as a receiving center from the lungs. The left atrium collects the oxygenated blood from the lungs and pushes the blood through the bicuspid valve into the left ventricle.
- Mitrol Valve: Named for the two flap nature of the valve. The valve is open during the diastole and blood passes through this valve from the atrium into the ventricle.
- Left Ventricle: The larger of the two ventricles, this part of the heart is more muscular than the right ventricle. It is responsible for pumping oxygenated blood through the entire body. Ventricles contract during the systolic phase of the heart and pump blood through the aortic valve.
- Aortic Valve: This valve opens during the systolic phase and allows blood to be pumped from the left ventricle into the Aorta.
- Aorta: The largest blood vessel in the body. The aorta acts like a junction where the freshly oxygenated blood flows through the body. The Aorta is separated into the ascending and descending Aorta. The ascending aorta supplies blood to the upper parts of he body, while the descending aorta supplies blood to the lower portions of the body. Apex: Distal point of the heart. An anatomical landmark that marks the bottom portion of the heart where the two ventricles meet.
- Septum: A fibrous barrier that separates the right and left ventricle.
- Pericardium: A fibrous membrane that encases the exterior of the heart. Peri meaning outer and cardium meaning heart.
- Myocardium: This is the name of the muscular structure of the heart. Myocardium literally means muscle of the heart. It is comprised of the muscles responsible for pushing the blood through the body.
- Endocardium: This is the fibrous membrane that lines the inside of the heart. It is smooth as to not cause rupture of red blood cells.
An EMT’s knowledge of the intricate electrical conduction system of the heart is indispensable. The heartbeat is coordinated by electrical impulses generated by this system, which also triggers the heart’s contractions. Any disturbance in this system can lead to arrhythmias, or irregular heart rhythms, which can be life-threatening if not treated immediately. A significant part of this system consists of two main nodes: the Sinoatrial (SA) node and the Atrioventricular (AV) node. Let’s explore these nodes and the heart rates typically associated with each.
Sinoatrial (SA) Node: The Heart’s Natural Pacemaker
The Sinoatrial node, or SA node, is often termed as the heart’s natural pacemaker. Located in the right atrium, it is responsible for initiating each heartbeat. The SA node generates electrical impulses that spread throughout the atria, causing them to contract and pump blood into the ventricles.
In a healthy adult at rest, the SA node fires between 60 to 100 times per minute. This is considered a normal resting heart rate. However, factors such as fitness level, emotional state, medication use, and age can influence this rate.
Atrioventricular (AV) Node: The Gatekeeper
Situated in the lower part of the right atrium, the Atrioventricular or AV node serves as a critical gateway in the heart’s electrical conduction system. It receives the electrical impulses from the SA node, delays them slightly to allow the ventricles to fill with blood, and then transmits them to the ventricles causing them to contract.
In the event of an SA node malfunction, the AV node can initiate electrical impulses on its own, but at a slower rate—usually between 40 and 60 beats per minute. This slower rhythm is often referred to as a junctional rhythm.
Beyond the Nodes: The Bundle of His and Purkinje Fibers
Once the electrical impulse leaves the AV node, it travels along the Bundle of His and then the Purkinje fibers, causing the ventricles to contract. If both the SA and AV nodes fail, these structures can also generate impulses, albeit at an even slower rate—around 20 to 40 beats per minute.
The Cardiac Cycle: A Journey Through the Heart
The cardiac cycle is an intricate sequence of events that takes place in the heart during one complete heartbeat. This vital process, occurring approximately 60 to 100 times per minute in a healthy resting adult, involves a series of coordinated contractions and relaxations of the heart chambers to pump blood throughout the body.
Two Phases of the Cardiac Cycle: Systole and Diastole
The cardiac cycle can be divided into two main phases: systole and diastole.
Systole: The Contraction Phase
Systole is the phase during which the heart contracts. It begins with the closure of the atrioventricular valves (tricuspid and mitral valves) to prevent backflow into the atria. This closure results in the first heart sound, often described as “lub.”
This phase is divided into two stages:
- Isovolumetric contraction: The ventricles start to contract, but the volume of blood within them remains unchanged as all the valves are closed.
- Ventricular ejection: The increased pressure within the ventricles forces the semilunar valves (pulmonic and aortic valves) to open, ejecting blood into the pulmonary artery and the aorta.
Diastole: The Relaxation Phase
Diastole is the phase during which the heart relaxes and fills with blood. It begins with the closure of the semilunar valves, preventing backflow into the ventricles, resulting in the second heart sound often described as “dub.”
This phase is divided into three stages:
- Isovolumetric relaxation: The ventricles begin to relax, but the volume of blood within them remains unchanged as all the valves are closed.
- Early ventricular filling: The pressure in the atria becomes higher than that in the ventricles, causing the atrioventricular valves to open and blood to flow into the ventricles.
- Atrial systole (late ventricular filling): The atria contract, pushing the remaining blood into the ventricles.
This systematic and rhythmical contraction and relaxation process of the cardiac cycle ensures the effective circulation of blood, providing oxygen and nutrients to the body’s tissues and organs.
Blood is transported throughout the body via an extensive and complex network of arteries, veins, and capillaries. Each is constructed and used in a different way. The oxygenated blood leaves the heart through the arteries, which are strong and durable. The veins carry the blood that has been deprived of oxygen back to the heart through one-way valves. Capillaries are the tiniest and most numerous blood vessels, and they play a key role in transporting oxygen, nutrients, and waste products from the circulatory system to the body’s tissues.
Blood is a unique bodily fluid that serves many important purposes. It’s crucial to our immune response and helps regulate temperature and waste removal, among other functions.
Why Dose an EMT Need to Know Cardiovascular Anatomy?
There are two primary reasons why EMTs need to have a solid understanding of the cardiovascular system. Heart-related emergencies occur frequently, to begin with. Intense chest pain, shortness of breath, and mental confusion are all symptoms that should alert a person to the possibility of cardiovascular disease. An EMT’s ability to recognize these symptoms and to interpret their potential meanings is critical because it informs their decisions and actions in the field.
Second, EMTs are frequently the first healthcare providers to engage with a patient in the “golden hour,” the period immediately following an emergency in which interventions can have the greatest possible effect on the patient’s outcome. This is especially true for those who suffer from cardiovascular disease. In the case of a heart attack, for instance, the damage can be permanent in a matter of minutes. If a patient receives a diagnosis and begins treatment quickly, their chances of survival and recovery are greatly increased.
Therefore, it’s not just helpful to have a good grasp of the cardiovascular system’s operations; it’s necessary. It lays the groundwork for identifying and handling many of the most common emergencies an EMT will encounter on the job. A healthcare provider’s ability to correctly diagnose a patient’s condition, begin effective treatment, and communicate this information to colleagues can literally be a matter of life and death.
Emergency Medical Technicians and the Most Frequent Heart Problems
A wide variety of cardiovascular conditions are common among the patients EMTs see in their role as first responders. Understanding the signs and symptoms of these diseases is essential in order to provide appropriate treatment in a timely manner. Heart attacks, arrhythmias, heart failure, and hypertension are just some of the most common cardiovascular emergencies seen by EMTs, and they will all be discussed in this section.

Heart Attacks (Myocardial Infarctions)
A heart attack, or myocardial infarction, is a life-threatening emergency that requires immediate medical attention. As an EMT Basic, your primary focus is to recognize the signs and symptoms of a heart attack and provide prehospital care to stabilize the patient while transporting them to the nearest appropriate medical facility. Let’s review the steps an EMT Basic can take to manage a suspected heart attack, including the use of oxygen, nitroglycerin, and baby aspirin.
Recognition and Initial Management
Recognizing a heart attack can be challenging, as symptoms can vary greatly among individuals. Classic symptoms include chest pain, shortness of breath, nausea, vomiting, sweating, and discomfort radiating to the jaw, neck, or arms. Women, in particular, may present with less typical symptoms, such as fatigue, dizziness, or abdominal discomfort. Always consider a heart attack in any patient presenting with chest discomfort or other signs suggestive of heart disease.
Initially, aim to comfort and reassure the patient. Minimize their physical activity and help them into a position that eases their discomfort—usually a semi-sitting position.
Oxygen Administration
Oxygen is crucial for patients suffering from a heart attack as it can help increase the amount of oxygen available to the heart muscle, which may be deprived due to blocked coronary arteries. Administer high-concentration oxygen (usually 15 liters per minute) via a non-rebreather mask.
Nitroglycerin Administration
If the patient has a prescription for nitroglycerin, and their blood pressure is within a safe range (usually systolic blood pressure above 90-100 mmHg), assist them in taking their medication. Nitroglycerin can help to dilate coronary arteries and improve blood flow to the heart muscle.
Always confirm with medical control or follow your local protocols before assisting with nitroglycerin administration, as there are contraindications, such as recent use of erectile dysfunction medications, to be aware of.
Baby Aspirin Administration
Chewable baby aspirin (typically four 81 mg tablets for a total of 324 mg) is often given to heart attack patients. Aspirin acts as an antiplatelet agent, reducing clot formation and helping to restore blood flow in the blocked artery.
Always ask about an allergy to aspirin or a history of gastrointestinal bleeding before administration and make sure the patient chews the aspirin for faster absorption. Again, follow your local protocols or obtain medical control clearance before administering aspirin.
Cardiac Monitoring and Rapid Transport
Monitor the patient’s vital signs closely and prepare for rapid transport to the hospital. If available and allowed by protocol, perform a 12-lead ECG. Time is crucial in a heart attack—every minute counts.
While EMT-Basics may not perform invasive procedures, their role in early recognition, initial management, and rapid transport of heart attack patients can have a significant impact on patient outcomes. Providing oxygen, assisting with nitroglycerin and aspirin administration, and facilitating rapid transport are all critical steps in the chain of survival for heart attack patients.
Arrhythmias
Arrhythmias represent abnormalities in the heart’s rhythm, triggered by issues within the heart’s electrical conduction system. Arrhythmias vary widely, from benign to severe. Symptoms can range from palpitations and fatigue to loss of consciousness or even cardiac arrest in extreme cases. Medication or implantable devices may be necessary for treatment, depending on the type and severity of the arrhythmia.
Heart Failure
Heart failure is a chronic condition where the heart can’t pump sufficient blood to meet the body’s demands. Tiredness, shortness of breath, swelling in the legs, and a racing heart could be symptoms. Although there is currently no cure for heart failure, it can often be controlled with medication and behavioral modifications.
Hypertension (High Blood Pressure)
Hypertension is when the blood’s force against artery walls is consistently too high. Untreated hypertension is associated with serious outcomes such as heart attack, stroke, and kidney disease, despite the fact that the condition is often asymptomatic in its early stages. Treatment focuses on controlling blood pressure through lifestyle modifications and medication.
The ability of EMTs to detect these heart conditions early on can have a significant effect on patient outcomes. For instance, recognizing the symptoms of a heart attack and starting treatment before getting to the hospital can reduce the amount of damage done to the heart and increase the chances of survival.
EMTs can better anticipate and manage emergencies by having a firm grasp on the potential complications associated with these conditions. Cardiac arrest can be the result of a heart attack or certain types of arrhythmia, making prompt EMT intervention crucial.
When you work as an EMT, you do so as part of a larger medical group. The patient will receive the best possible follow-up care and treatment if the emergency room and other healthcare providers have access to accurate and timely information.
Cardiovascular Patient Assessment for EMTs
Emergency Medical Technicians (EMTs) are often the first healthcare professionals on the scene of a medical emergency. Assessing and diagnosing cardiovascular conditions quickly and accurately can have a major effect on patient outcomes. The electrocardiogram (ECG) is one example of a diagnostic tool that is used by paramedic level providers. As an EMT you will need to rely on your patient assessment skill and ability to identify key symptoms in order to determine if your patient is having a cardiac emergency.
Patient Interview: The First Step
An essential part of the EMT’s evaluation is the initial conversation with the patient. During this exchange, EMTs can ask the patient and any witnesses present for crucial details about their condition. First, EMTs must determine the patient’s “chief complaint,” or the primary ailment that prompted them to call for help. Symptoms of a heart problem may include discomfort in the chest, difficulty breathing, dizziness, and fatigue.
Next, EMTs investigate the patient’s history of the present illness (HPI), which is a thorough description of the onset and evolution of the symptoms. Performing such an investigation can help doctors better understand the patient’s condition and its severity.
The patient’s medical history is also recorded by the EMT, with special focus on the presence or absence of cardiovascular disease. The last thing the patient ingested orally (whether it was food, liquid, or medication) can help the EMT predict potential complications and determine the best course of treatment.
The EMT’s ultimate goal is to determine what precipitated the current illness. Consider the patient’s activity level, mental health, environmental stresses, and any other relevant factors. The EMT can gain valuable insight from this background information as they investigate potential causes of the symptoms.
Physical Examination: Key Observations
Once the EMT has finished talking to the patient, they will perform a physical examination. In the first phase of this checkup, the examiner will form an overall impression of the patient based on their demeanor, gait, and skin condition. All abnormalities that may indicate a problem will be investigated by EMTs.
The following important indicators are blood pressure, heart rate, respiratory rate, and oxygen saturation. Each of these readings has the potential to shed light on the patient’s cardiovascular health and reveal any impending crises.
The next step is a more in-depth physical examination, during which the doctor may use a stethoscope to listen to the patient’s heart and lungs, look for signs of poor circulation on the skin (such as pallor, coolness, or bluish tint), and check for swelling in the legs and ankles, which may indicate heart failure.
Finalizing the Evaluation and Transfer
The EMT can then formulate a primary impression based on the collected data. The EMT’s initial assessment of the patient’s symptoms serves as a starting point for determining the most appropriate course of treatment and can be revised as new information becomes available.
Transferring the patient to the hospital marks the completion of the process. The EMT gives a handover, which is a report detailing their findings and the care they gave the patient in a clear and concise format. The continued success of the hospital’s care delivery depends on this data.
In conclusion, the successful management of cardiovascular conditions relies heavily on thorough evaluation and correct diagnosis. The ability of EMTs to quickly gather and interpret information is crucial, as it will direct their interventions and potentially save the patient’s life.

Michael
Hey there! It's so great to meet you! My name is Mike, and I am thrilled to be able to share my extensive EMS experience with you. I am currently working as an EMT in Tucson and am also an EMT instructor at Pima Community College. I am passionate about teaching future first responders, and I created this site specifically to assist anyone interested in pursuing a career in EMS.
It's possible that you are here because you're considering becoming an EMT, or maybe you are already one. Throughout my career, I have tested out countless pieces of EMT-related gear and equipment, and I want to help guide you in making smart decisions when it comes to selecting the best gear for your needs.
I am here to offer my support, so feel free to reach out if there is anything you need. Let's work together to make sure you have the tools you need to excel in this rewarding field!
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on X (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to print (Opens in new window)
- Click to email a link to a friend (Opens in new window)