This article is for informational purposes only and is NOT a replacement for proper education and training.
Table of Contents
Overview and Function of EMTs in Neurological Emergencies
Emergency Medical Technicians (EMTs) frequently face difficult situations when responding to neurological emergencies, which are an essential component of emergency medical services. Rapid recognition and appropriate intervention in these circumstances can have a substantial impact on patient outcomes.
What are Neurological Emergencies?
Neurological emergencies are conditions affecting the nervous system that necessitate immediate medical care. Trauma, stroke, infection, and other underlying medical conditions are just a few possible causes of these medical emergencies. They may manifest as altered mental status, weakness or paralysis, seizures, sensation loss, or any other neurological deficit.
Strokes, traumatic brain injuries, seizures, and meningitis, among others, are typical examples of neurological emergencies. Each condition has distinct symptoms, and it is frequently the responsibility of EMTs to recognize these symptoms quickly and administer timely care.
The Role of an EMT in Neurological Emergencies

In any neurological emergency, the role of an EMT transcends that of a mere first-aid responder. They are the frontline soldiers in the race against time, and their primary responsibilities include ensuring the safety of the scene, performing an initial assessment, administering immediate care, and preparing for a rapid transport to the hospital.
Assessing the patient’s airway, breathing, and circulation—the ABCs—are often part of the EMT’s initial evaluation. After securing these, EMTs conduct a more focused neurological assessment. Key components include evaluating the patient’s level of consciousness, pupil reaction, and motor and sensory functions. Additionally, EMTs collect a thorough medical history, which provides context for the current emergency.
EMTs must keep in mind that the primary objective of managing neurological emergencies is to prevent further neurological damage and initiate treatment as soon as possible. This is where neurological assessment techniques become crucial, allowing EMTs to identify neurological deficits, anticipate complications, and guide their interventions.
We will delve deeper into the nervous system, its functioning, common neurological emergencies, and crucial assessment techniques every EMT should be proficient in. Our journey ahead will explore the complexities of neurological emergencies and the pivotal role of EMTs in managing them.
With knowledge, practice, and commitment, EMTs can strive to make a significant difference in the lives of their patients, serving as vital links in the chain of survival during neurological emergencies. Join us as we explore the fascinating world of neurology in emergency medical services, and let’s make a difference with each patient
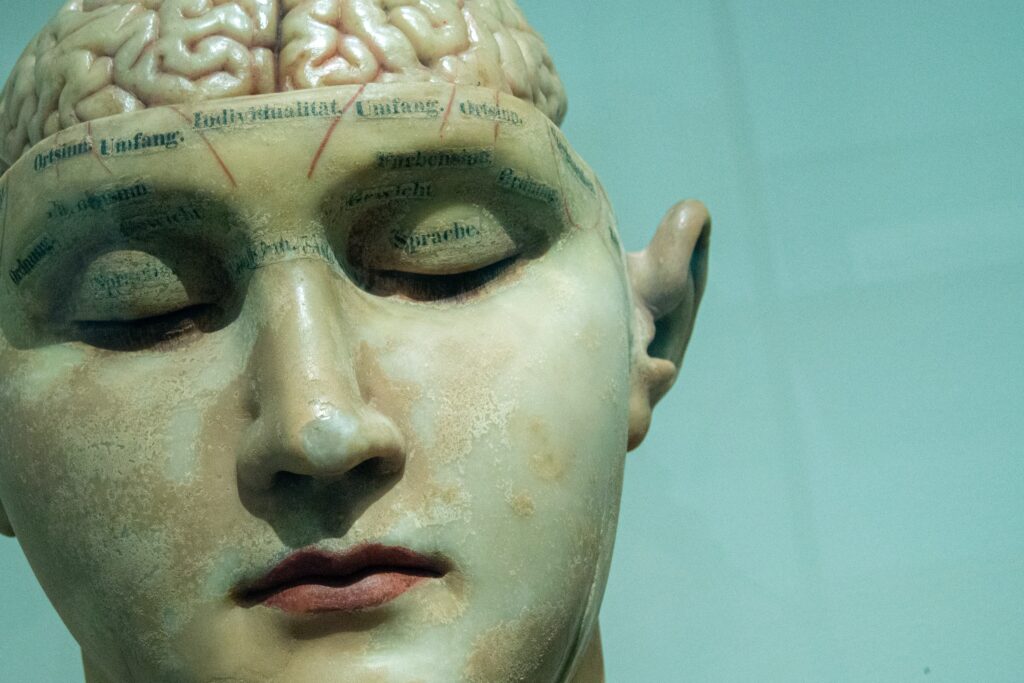
Understanding the Nervous System for EMTs
The nervous system, a complex network that serves as the body’s command center, is essential for managing neurological emergencies effectively. Emergency Medical Technicians (EMTs) must have a thorough knowledge of the nervous system and its functions in order to provide optimal care.
Introduction to the Nervous System
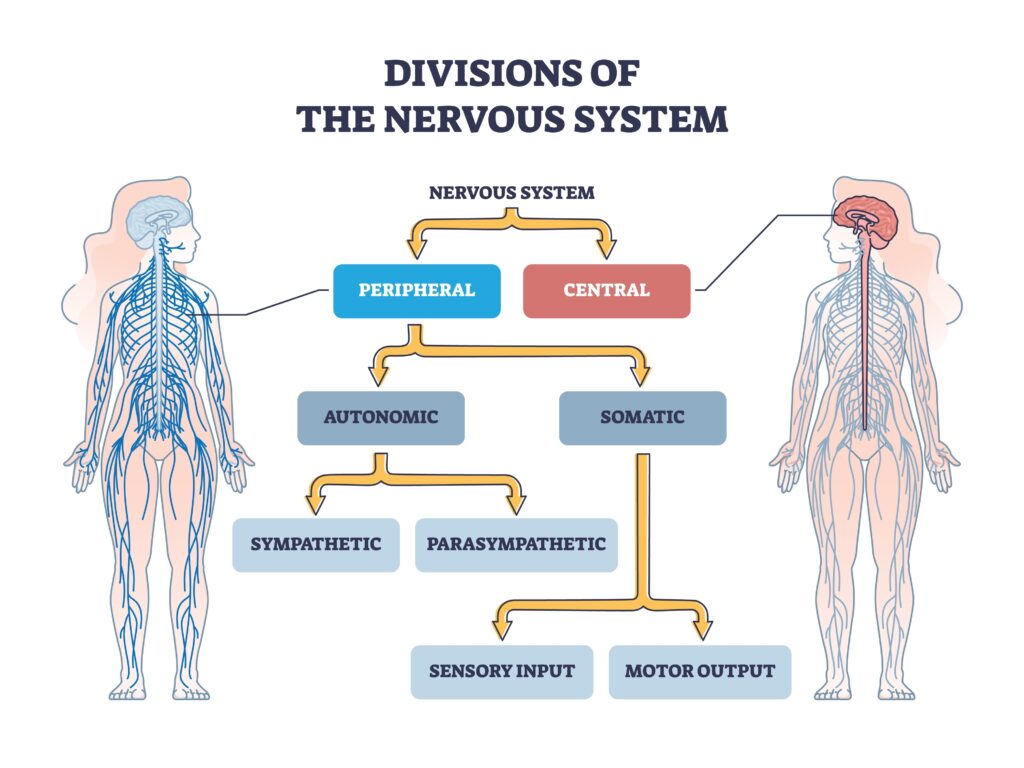
The nervous system consists of the Central Nervous System (CNS) and the Peripheral Nervous System (PNS). This classification is essential for comprehending the symptoms of various neurological disorders, as each system regulates distinct bodily functions.
Central Nervous System (CNS): The Control Center
The central nervous system consists of the brain and spinal cord. It functions as the command center, receiving information from the body and transmitting orders. Each region of the brain is responsible for specific functions:
- The cerebrum, the largest portion of the brain, is responsible for voluntary actions, speech, thought, and processing of sensory information.
- The cerebellum regulates balance and coordinates movement.
- The brainstem regulates automatic bodily processes such as respiration, heart rate, and blood pressure.
The spinal cord transmits signals in both directions between the brain and the rest of the body, acting as a relay station.
Peripheral Nervous System (PNS): The Communication Network
All nerves outside the CNS that transmit information to and from the brain and spinal cord comprise the PNS. The nervous system is subdivided into the somatic and autonomic nervous systems.
- The somatic nervous system regulates voluntary movement and relays sensory data to the central nervous system.
- The autonomic nervous system regulates involuntary functions such as heart rate and digestion, and is comprised of the sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems.
Understanding these systems and their functions can greatly assist EMTs in identifying and treating neurological emergencies.
How Neurological Conditions Affect the Nervous System
Damage to parts of the nervous system, affecting their functions, is frequently the cause of neurological disorders. For instance, a stroke can cause damage to the cerebrum, resulting in symptoms such as weakness, speech difficulties, and changes in sensory perception. A spinal cord injury may impact the motor and sensory functions below the injury site. A disease affecting the PNS could result in muscle deterioration and sensory alterations.
Understanding the functions of the brain and spinal cord, as well as their connections to the PNS, will enable EMTs to conduct more targeted neurological evaluations, identify abnormalities, and anticipate potential complications. This comprehension is essential for providing effective emergency care.
This information, coupled with a thorough understanding of the nervous system, will prepare EMTs for a wide variety of neurological emergencies, thereby enhancing their ability to provide effective and timely care.
As we continue to delve deeper into the fascinating world of neurology, keep in mind that as EMTs, your knowledge and skill in this field can have a significant impact on patient outcomes. Step by step, let’s continue this journey of learning and progressing together.
Key Neurological Assessment Techniques for EMTs
As an Emergency Medical Technician (EMT), competence in neurological assessment techniques is indispensable. It allows EMTs to quickly recognize neurological deficits, direct their interventions, and contribute to the optimal care of patients experiencing neurological emergencies. This article examines the essential assessment tools that should be part of every EMT’s toolkit.
Glasgow Coma Scale (GCS)
The GCS evaluates three key areas: eye opening, verbal response, and motor response. Each area is assessed separately and given a score. The total score, a sum of the three, ranges from 3 to 15. Lower scores indicate a more severe injury or impaired consciousness.
Eye Opening (E)
Evaluate how and when the patient’s eyes open.
- Spontaneous – 4 points
- To voice – 3 points
- To pain – 2 points
- No response – 1 point
Verbal Response (V)
Assess the patient’s ability to communicate. Be aware that this can be challenging with intubated patients.
- Oriented – 5 points
- Confused, but able to converse – 4 points
- Inappropriate words or phrases – 3 points
- Incomprehensible sounds – 2 points
- No response – 1 point
Motor Response (M)
Evaluate the patient’s ability to follow commands and respond to stimuli.
- Obeys commands – 6 points
- Localizes to pain – 5 points
- Withdraws from pain – 4 points
- Abnormal flexion to pain (decorticate posturing) – 3 points
- Abnormal extension to pain (decerebrate posturing) – 2 points
- No response – 1 point
The assessment should be performed methodically, and the patient’s score should be documented and communicated effectively to the entire healthcare team. If a patient has a GCS of 8 or less they are a critical patient and require immediate transport. As the medics like to say, “Less than 8 intubate”.
AVPU Scale
AVPU is an acronym that stands for Alert, Verbal, Painful, and Unresponsive, and it’s a simple and quick method for assessing a patient’s level of consciousness. Here’s a step-by-step guide on how to assess AVPU for Emergency Medical Technicians (EMTs).
Alert (A)
First, determine if the patient is alert. This means that the patient is fully awake (not necessarily oriented) and has spontaneous eye-opening. They should be able to respond appropriately to questions and be aware of their surroundings.
Verbal (V)
If the patient is not alert, determine if they respond to verbal stimuli. This could be a simple command, such as “Open your eyes,” or a question, “Can you tell me your name?” Remember, this is about the patient’s ability to respond, not necessarily to answer correctly or coherently.
Painful (P)
If there’s no response to verbal stimuli, you should check the patient’s response to painful stimuli. Use a universally accepted technique such as a sternal rub, a trapezius squeeze, or pressing on a fingernail bed. A responsive patient will grimace, pull away, or respond verbally to the stimulus.
Unresponsive (U)
If the patient doesn’t respond to painful stimuli, they’re classified as unresponsive. This is the most serious level of consciousness. Any patient who is unresponsive, or whose level of consciousness is rapidly declining, should be managed as a medical emergency.
Remember, AVPU doesn’t provide a detailed neurological assessment, but it is a quick and useful tool for an initial assessment of a patient’s level of consciousness. It can be particularly useful in emergency situations or for a quick re-assessment of a patient’s condition.
The AVPU scale is widely used in prehospital settings, and becoming proficient in its use will help you quickly recognize patients with potentially life-threatening levels of altered mental status.
Pupil Evaluation
The pupils can provide invaluable insights into a patient’s neurological status, particularly in conditions such as head injuries, strokes, and certain systemic illnesses. Read on for a guide on how to perform a pupillary assessment.
Equipment
For a pupillary assessment, you will need a source of light, typically a flashlight or a penlight.
Pupil Size
Begin your assessment by observing the size of the patient’s pupils. They may be pinpoint, normal, or dilated. In a normal state, the pupils are equal in size, a condition known as “equal, round, and reactive to light and accommodation” (ERRLA).
Pupil Shape
Next, note the shape of the pupils. They should be round. An irregular shape can be a sign of trauma or neurological abnormality.
Pupil Equality
Compare the pupils to each other to evaluate their equality, a condition known as equality or isocoria. If one pupil is significantly larger than the other, it’s a condition known as anisocoria, which can be a sign of a serious condition like a brain herniation.
Pupil Light Reflex
To assess the pupil light reflex, darken the room if possible, then shine a light into each pupil. In a normal response, the pupil will constrict, or get smaller, when the light is shone on it, known as direct response. The other pupil should also constrict when the light is shone in the opposite pupil, known as consensual response.
Pupil Accommodation
Assessing accommodation involves observing the pupils as the patient focuses on a distant object and then on a near object. In a normal response, the pupils will constrict when the patient focuses on a near object.
It’s important to remember that the pupils are just one piece of the neurological assessment. They should be evaluated in conjunction with other assessments like the Glasgow Coma Scale (GCS) or AVPU. Also, changes in pupillary response can indicate a change in the patient’s condition, highlighting the importance of repeated assessments.
Motor and Sensory Assessment
The motor assessment evaluates muscle strength, muscle tone, and coordination. Assessing a patient’s ability to voluntarily obey commands and move limbs Evaluation of the patient’s senses of touch, pain, temperature, and position comprise the sensory assessment. Abnormalities may be indicative of problems in particular regions of the brain, spinal cord, or peripheral nerves.
These evaluations can provide invaluable information about the neurological status of the patient, allowing for informed decisions and targeted care.
The Role of Medical History in Neurological Assessment
EMTs should collect a comprehensive medical history, which provides context for the patient’s presenting symptoms and aids in determining the patient’s neurological status. Important details include preexisting neurological conditions, medications, the onset of symptoms, and any recent trauma, illness, or unusual events. A thorough medical history can frequently reveal the underlying cause of a neurological emergency.
Mastering neurological assessment techniques can significantly enhance an EMT’s capacity to manage neurological emergencies. These tools enable EMTs to rapidly identify neurological deficits, direct their interventions, and transmit vital information to the receiving hospital.
Nevertheless, keep in mind that learning these skills is only the beginning. The only way to truly incorporate these skills into your EMT routine and instincts is through consistent practice and application in the field. By doing so, you will be better equipped to deal with neurological emergencies and have a significant impact on the lives of your patients.
Real-life Applications of Neurological Assessment Techniques for EMTs
In order to manage neurological emergencies, Emergency Medical Technicians (EMTs) must first understand neurological assessment techniques. The true challenge lies in implementing these techniques in real-world scenarios. We will discuss the use of these techniques in common neurological emergencies such as Traumatic Brain Injury (TBI), stroke, and seizures.
Traumatic Brain Injury (TBI)
TBIs are common neurological emergencies, often resulting from motor vehicle accidents, falls, or violent assaults. To assess the patient’s level of consciousness, EMTs should perform the Glasgow Coma Scale and the AVPU scale immediately.
Evaluation of the pupils is essential in traumatic brain injuries, as unequal pupils or pupils that do not react to light may indicate increased intracranial pressure or brain herniation, both of which are fatal conditions. The evaluation of motor function identifies any weakness or paralysis, which may indicate a localized brain injury.
Stroke (CVA)
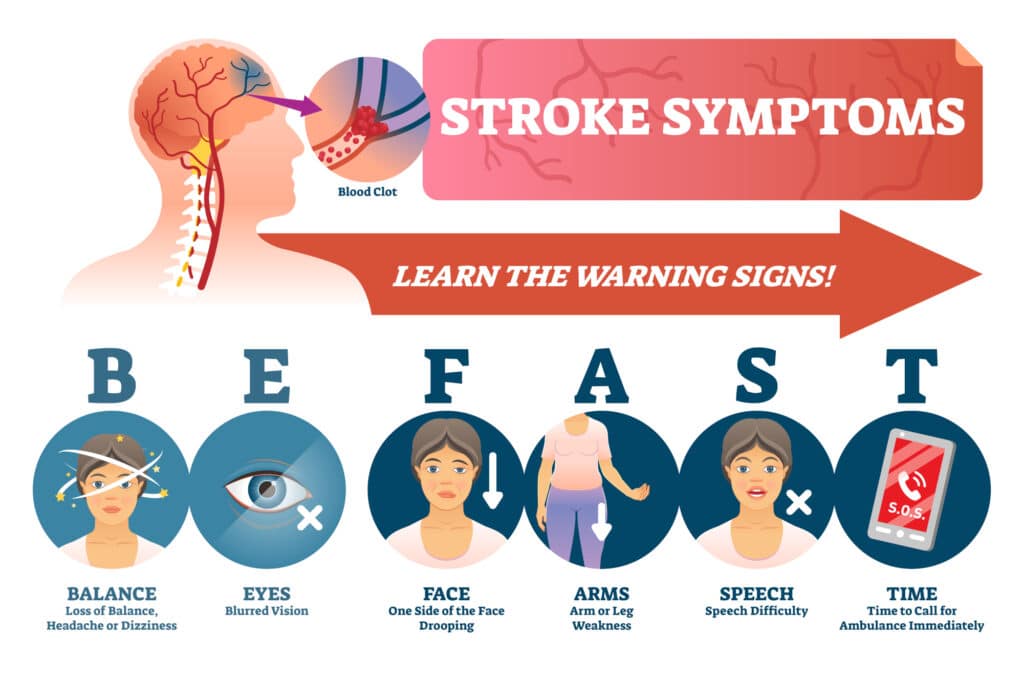
In patients with a stroke, time is brain. Rapid recognition and transport to a stroke center can substantially improve patient outcomes. EMTs can identify potential stroke victims using tools such as the Cincinnati Prehospital Stroke Scale and the FAST (Face, Arm, Speech, Time) exam.
In addition, a comprehensive neurological evaluation, including GCS, pupil evaluation, and motor and sensory evaluations, is required. These assessments can help determine the severity of the stroke and its possible location in the brain, allowing the hospital staff to prepare for immediate treatment.
Seizure
An EMT’s primary responsibility when encountering a patient with seizures is to ensure the patient’s safety, manage the airway, and administer authorized medications. After a seizure, it is essential to conduct a complete neurological evaluation. Changes in level of consciousness, abnormal pupil reactions, or new motor or sensory deficits may indicate a more serious underlying cause for the seizure, such as a brain tumor or a stroke.
The Importance of Neurological Evaluations in Patient Transfers
During patient transfer, it is crucial to relay accurate results of neurological evaluations. It gives the receiving healthcare team a clear picture of the patient’s neurological condition and any changes that occurred during prehospital care.
Remember, although the initial focus in neurological emergencies is frequently the ABCs (Airway, Breathing, Circulation), a thorough neurological assessment should never be neglected. The earlier neurological deficits are identified, the sooner appropriate interventions can be initiated, and the more favorable the prognosis for the patient.
With consistent practice, these assessment techniques will become second nature, allowing you to provide optimal care for your patients during neurological emergencies.
The Importance of Neurological Assessments in Prehospital Care: A Review and Reflection
In this article, we have explored the intricate world of neurological emergencies and the role of Emergency Medical Technicians (EMTs) in their management. Let’s wrap up by reviewing and reflecting on the significance of neurological assessments in prehospital care.
The Pivotal Role of EMTs in Neurological Emergencies
As EMTs, you are frequently the first medical responders to patients with neurological emergencies. Your prompt recognition of neurological deficits and initiation of appropriate interventions can have a significant impact on a patient’s prognosis.
The initial management of common neurological emergencies such as Traumatic Brain Injury (TBI), stroke, and seizures is highly dependent on your ability to conduct a comprehensive and accurate neurological assessment.
A Review of Neurological Assessment Techniques
The Glasgow Coma Scale (GCS), the AVPU scale, pupil evaluation, and motor and sensory assessments were explored in detail. These techniques assist in determining the presence and severity of neurological deficits, guiding your interventions, and providing valuable information to the receiving hospital team.
Don’t forget that each assessment technique has its own place in prehospital care. While tools such as GCS and AVPU are essential in any neurological emergency, the value of more targeted evaluations such as pupil evaluation and motor and sensory evaluations should not be undervalued.
Reflection on Real-Life Applications
Real-world application of these techniques is both difficult and rewarding. Assessing the GCS of a patient with a TBI at a chaotic accident scene or identifying stroke symptoms in a distressed patient can be stressful. Nevertheless, your knowledge and prompt actions can significantly improve the prognosis for these patients, demonstrating the impact EMTs can have in neurological emergencies.
The Importance of Continual Learning and Development
As an EMT, your education is ongoing. With each interaction, you gain experience and hone your abilities. Regular review and practice of these neurological assessment techniques, as well as keeping abreast of the most recent prehospital care recommendations, can increase your competency and confidence in managing neurological emergencies.
To provide the best patient care, you must reflect on your experiences, learn from your challenges, and strive to continually improve your skills. Your dedication and commitment can make a significant difference in the lives of your patients.
As we conclude our article on neuropsychological evaluations for EMTs, we hope that you have gained valuable knowledge and skills. Remember that your role as an EMT is invaluable in the world of neurological emergencies. Effective assessment, intervention, and communication can have a significant impact on patient outcomes. Therefore, let’s continue to learn, improve, and strive to provide the best care possible to our patients, one neurological evaluation at a time.

Michael
Hey there! It's so great to meet you! My name is Mike, and I am thrilled to be able to share my extensive EMS experience with you. I am currently working as an EMT in Tucson and am also an EMT instructor at Pima Community College. I am passionate about teaching future first responders, and I created this site specifically to assist anyone interested in pursuing a career in EMS.
It's possible that you are here because you're considering becoming an EMT, or maybe you are already one. Throughout my career, I have tested out countless pieces of EMT-related gear and equipment, and I want to help guide you in making smart decisions when it comes to selecting the best gear for your needs.
I am here to offer my support, so feel free to reach out if there is anything you need. Let's work together to make sure you have the tools you need to excel in this rewarding field!
Share this:
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on X (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on Mastodon (Opens in new window)
- Click to print (Opens in new window)
- Click to email a link to a friend (Opens in new window)