Physiology of the Heart:
It is important for EMTs and Paramedics to have an understanding of the anatomical structure of the heart. However, they must also possess an intimate understanding of the function of the myocardium. The purpose of this page will be to provide study notes on the following: The Cardiac Cycle, Nervous Control of the Heart, and an understanding of the Chemicals and Electrophysiology of the central pumping mechanism of the body. These notes DO NOT replace classroom instruction or home study courses but are intended to supplement them in an easy to access and easy to study format. They form a distillation of the information to the important aspects. Students are encouraged to look into additional study materials. This page is useful to EMTs as well as those attending Paramedic level classes.
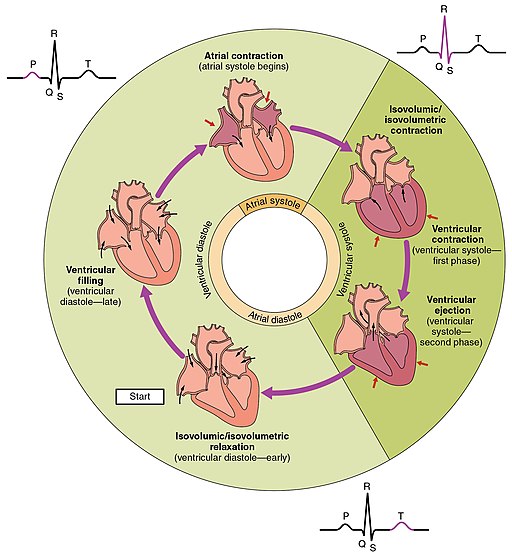
The Cardiac Cycle:
The cardiac cycle describes the life sustaining sequence of events that take place within the heart to pump blood throughout the body. There are a large amount of events and factors that have to happen in order for our heart to go from a organ made of meat and blood vessels to a functioning bio-organic pump fueled by chemistry and electricity. The heart has two phases:
Diastole:
First phase of the cardiac cycle. Blood begins entering the ventricles from the atria. The heart is at rest and the coronary arteries oxygenate the heart at this point. Mitral and Tricuspid valves are open (allowing blood into the ventricles). Aortic and Pulmonic Valves are closed(preventing back flow into the ventricles).
Systole:
Second phase of the cardiac cycle. The heart is active. Blood is pumped into the lungs through the Pulmonic Valve and into the aorta through the Aortic Valve. Just before the closure of the Mitral and Tricuspid Valves, the Atria contract and force the remaining blood into the ventricles. During Ventricular contraction the Atrial Valves close, preventing back flow and ensuring that the ventricular contraction forces the blood either into the lungs or the aorta.
Mechanics of a Heartbeat:
When the ventricles contract during systole they eject roughly two thirds of the blood they contain by the end of the systolic phase. This is the ejection fraction. The amount of blood ejected is known as the stroke volume.
Ejection Fraction:
A healthy heart has an ejection fraction of 2/3 the blood contained in the ventricle.
Stroke Volume of the Heart:
The amount of blood the heart ejects into the aorta. Normally between 60 and 100 ml. Average is 70 ml.
Important Terms of Note:
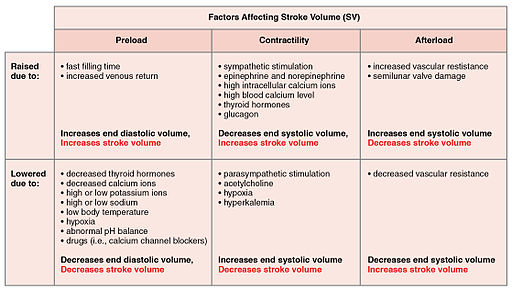
Preload:
Amount of blood left in the ventricle after systole. Factors in the force and volume of next contraction.
Afterload:
The vascular resistance that the ventricle has to push against during contraction. Higher resistance lowers stroke volume and lower resiatnce increases stroke volume.
Starling’s Law of the Heart:
This law states that the more the cardiac muscle is stretched the more forceful the contraction will be. Think a rubber band, the more it is stretched the harder it will snap back. The cardium has its limits and if stretched too much (for instance to meet the demands of increased cardiovascular resistance) the ability to pump is impacted as the heart can lose elasticity. The greater the venous return to the heart the great the contractile force will be. More venous blood increases preload and stroke volume. Like filling a balloon with water. The more water in the balloon the more force it will be expelled with when pressure is released.
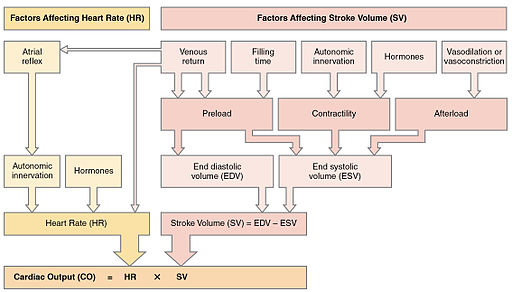
Cardiac Output:
Amount of blood pumped in 1 minute.
Cardiac Output Calculation:
Stroke Volume (mL) x Heart Rate (bpm) = Cardiac Output (mL/min)
Average Cardiac Output:
5000 mL/min
Blood Pressure Equation:
Cardiac Output x Systemic Vascular Resistance
Note on Blood Pressure:
Body keeps BP in a state of homeostasis. Increases and decreases vascular resistance to maintain a mean blood pressure.
Other Notes:
Important to study these formulas. An audio study program can aid in retaining this information. These can be listened to while at the gym or on the way to work in the car.
test section
How the Heart is Controlled Via the Nervous System:
The heart, like the rest of the body, is affected by both the sympathetic and parasympathetic nervous systems. These systems are in direct conflict with each other and function in a push pull manner to achieve homeostasis.
Heart Nervous Receptors:
These receptors receive information from neurotransmitters and each receptor site has an effect on the actions of the heart, lungs, and cardiovascular system. An easy trick to remember what receptors effect which in regards to the Beta Receptors: You have 1 heart and 2 lungs. Beta 1 affects the heart, Beta 2 affects the lungs.
Beta 1:
Located in the heart. Increase heart rate and contractile force.
Beta 2:
Located in the lungs and peripheral blood vessels. Cause bronchial dilation and vasodilation of the peripheral vasculature.
Alpha 1:
Located in the blood vessels. They cause vasoconstriction.
Sympathetic Nervous System Effects on the Heart:
Also known as the Fight or Flight nervous system. This nervous system takes over during stressful situations. The sympathetic nerves connect the heat at the base of the cardium and are known as the Cardiac Plexus. They are connected from the thoracic and lumbar regions of the spine. The neurotransmitter for the sympathetic system is NorEpinephrine. The effects of the sympathetic nervous system include increased heart rate and increased cardiac contractile force. NorEpi effects beta receptors.
Parasympathetic Nervous System Effects on the Heart:
Also known as the feed and breed portion of the nervous system. Using the neurotransmitter acetylcholine, the parasympathetic nervous system slows the heart rate and atrioventricular conduction. acetylcholine stimulates receptors on the vagus nerve . The vagus nerve is the principal parasympathetic nerve that innervates the heart. The connect to the heart mainly at the atrial sites. The vagus nerve is also the 10th cranial nerve.
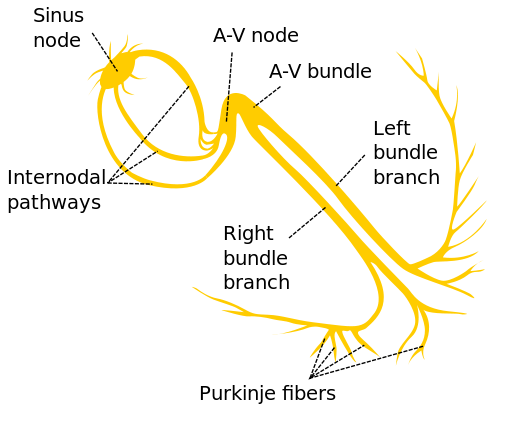
Electrophysiology of the Heart
The heart has its own electrical system. This is how the heart functions. Electricity stimulates muscles. Muscles contract and blood is pumped through the circulatory system. The process is far more complex than how electricity is powering the device you are reading these notes on. The heart is a bio-electrical pump. This means the electricity is created through organic means. As you can see from the picture. The heart, like a house, has its own wiring system.
Spark Plugs of the Heart – SA Node, AV Node, Purkinje Fibers
SA Node:
Sinoatrial Node. Principal pacemaker of the heart. Starts the electrical process of the heart. Intrinsic rate: 60-100 beats per minute. First to fire fastest intrinsic rate. Produces a sinus rhythm on an EKG
AV Node:
Atrioventricular Node. Secondary pacemaker of the heart, Think of it like a back up. It is connected to the SA Node through Intranodal pathways. If the SA node fails to fire the AV node is the next in line. However it has a slower intrinsic rate. Intrinsic rate: 40-60 beats per minute. Produces a junctional rhythm on an EKG.
Purkinje System:
This is the tertiary ignition system of the heart. The last line of defense. These are they guys that stayed at the alamo. Should the SA and AV node fail to fire then the Purkinje Fibers set the pace of the heart. Electricity travels the slowest through these fibers. Intrinsic Rate: 15-40 beats per minute. Produces a ventricular rhythm on an EKG.
How the Heart Beats:
Electrolytes:
Muscles contract based upon bioelectricity. Electrolytes are the stimulus that enable electrical conduction. Notice the name ELECTROLYTES. ELECTRO. Electricity. The heart, being a muscle, relies on the chemical ions known as electrolytes to function.
Electrolytes Include:
- Sodium (Na+)
- Has a role in depolarization of the myocardium
- Calcium (Ca++)
- Has a role in depolarization and the actual contraction of the heart.
- Potassium (K+)
- Has a role in repolarization of the myocardium
- Chloride (Cl-)
- Helps maintain proper acidity
- Magnesium (Mg++)
- Maintains stability such as heart rate, and facilitates communication between nerves and muscles.
Function of Cardiac Muscle
Heart muscle function begins at the cellular level. Cardiac muscle is special in that it is striated like the muscles in the arms or legs, that is controlled through conscious thought. However it is a muscle that functions without conscious thought like smooth muscles, such as those in the blood vessels.
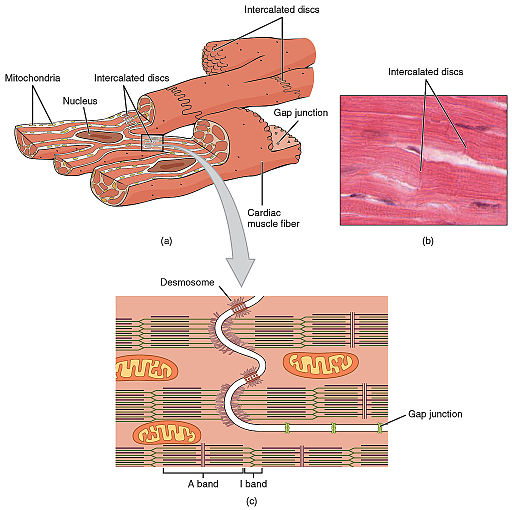
Cardiac muscle comes in a couple varieties: Atrial, Ventricular, and with specialised excitatory and conductive muscle fibers. A key feature to cardiac muscle cells are the intercalated discs. This is where cardiac muscle differs from skeletal muscle. While they function the same, the intercalated discs conduct electrical impulses 400 times faster than typical skeletal muscle. This is the key that allows for the heart to contract as one unit. One cell becomes excited and contracts and the rest follow so fast that the heart could be seen as one giant cell.
The heart has two areas that work this way. These area’s of hypercontractivity. Atrial and Ventricular. This unit is called syncytium. The atrial syncytium contracts superior to inferior. The ventricular syncytium contracts the opposite way. Inferior to superior.
Atrium: Top to Bottom.
Ventricle: Bottom to Top.
Key Aspects of Cardiac Electrophysiology
Cardiac Depolarization:
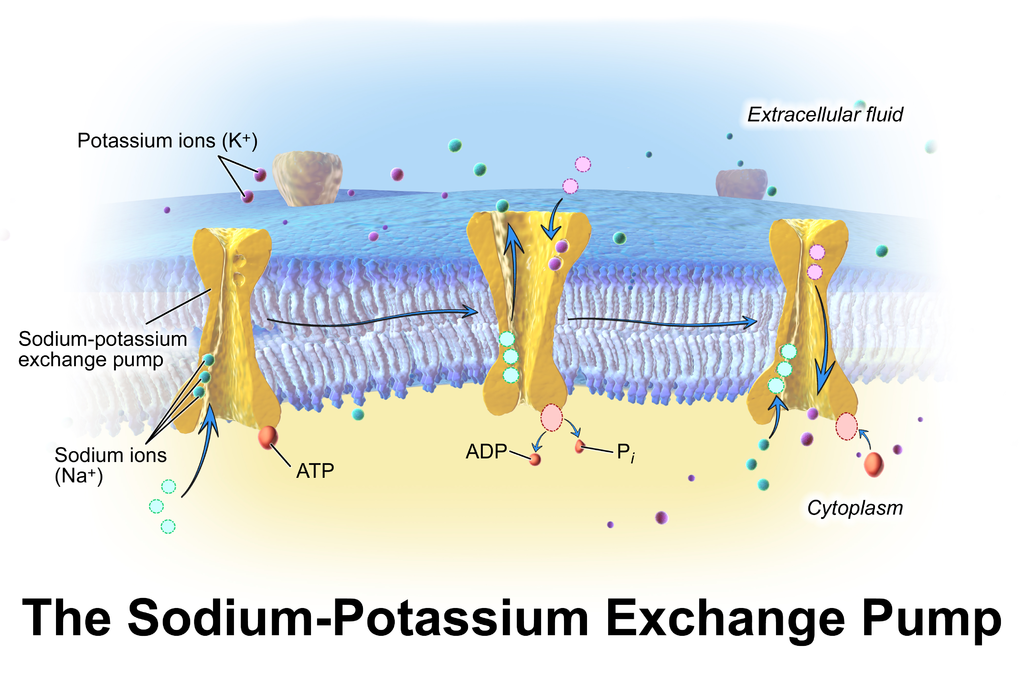
The key to Cardiac Muscle Depolarization lays in the Sodium-Potassium pump. The pump expels 3 sodium (Na+) cations out of the cell and only allows 2 potassium (K+) cations back into the cell while the pump is open. Inside of cell is left negatively charged in relation to outside of the cell.
The imbalance is called the Resting Potential. The Resting Potential is when the inside of the cell is more negatively charged than the outside of the cell. Resting potential of the cardiac cell is approximately -70mV.[/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]